Introduction
As people with sickle cell disease (SCD) age, they experience accelerated functional decline. Since historically survival for SCD has been limited to middle age, geriatric syndromes in adults with SCD remains understudied. Chronological age does not accurately represent a person's health status; thus, valid functional measures for adults with SCD are required. Geriatric assessments are commonly used to measure function in older adults in the general population. We previously demonstrated feasibility, safety, and acceptability of a geriatric assessment battery called the Sickle Cell Disease Functional Assessment (SCD-FA) in adults with SCD. The SCD-FA includes physical performance test and surveys evaluating multiple health domains. The purpose of this study was to evaluate the construct validity of the SCD-FA.
Methods
We enrolled younger (age 18-39) and older (age ≥ 40 years) adults with SCD in a single center prospective study. We assessed construct validity of each SCD-FA measure by determining known-group validity. Specifically, we evaluated whether the SCD-FA could distinguish between participants known to differ based on the following: age (< 40 vs ≥ 40), SCD genotype non-severe (HbSC/HbSβ +-thalassemia) vs severe (HbSS/HbSβ 0-thalassemia), and dependence in Activities of Daily Living/Instrumental Activities of Daily Living (no ADL/IADL deficit vs ≥ 1 ADL/IADL deficits). We used Student's t-tests and Wilcoxon rank sum test to gauge significant differences between groups.
Results
We performed the SCD-FA in 111 adults with SCD at steady state, with 93 (84%) having complete data. Most participants (58%) were female.
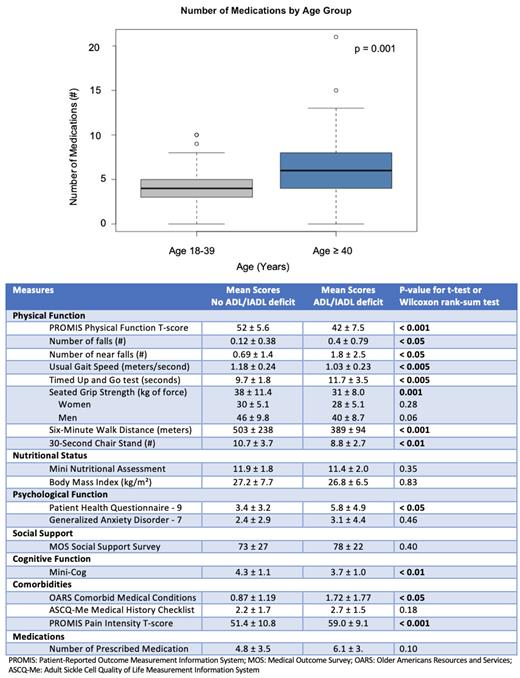
The mean age of all participants was 44 ± 14 (range 19-82 years), with most (56%) age ≥ 40 years. The mean age for younger adults (18-39 years) was 30 ± 5.8 and 54 ± 9.3 for older adults (≥ 40 years). When evaluating SCD-FA measures by age, older adults had lower scores on PROMIS Physical Function (younger 52 ± 6.9 vs older 46 ± 8.4; p<0.001). Although there was no difference in number of falls by age, there were several participants with ≥ 1 fall (15%) or near fall (36%) in the last 6 months. Older adults had higher scores on the Social Support Survey (implying better support) (younger 69 ± 30 vs older 80 ± 20; p< 0.05). Older adults had more non-SCD comorbidities (younger 0.5 ± 0.7 vs older 1.7 ± 1.7; p<0.001), with no younger adults with ≥ 3 comorbidities vs. 33% of older adults with ≥ 3 comorbidities, more SCD conditions (younger 2.0 ± 1.5 vs older 2.7 ± 1.7; p< 0.05), and more reports of fair or poor hearing (0% younger vs 8% older; p = 0.01). Older adults took more prescribed medications (younger 3.9 ± 2.4 vs older 6.3 ± 3.9; p = 0.001) and were more likely to meet criteria for polypharmacy (defined as ≥ 5 prescribed medications) with 30% of younger adults vs 64% of older adults (Figure).
Most participants (64%) had HbSS/HbSβ 0 (severe genotype) and 36% had HbSC/HbSβ + (non-severe genotype). When comparing groups by genotype, participants with severe genotypeshad a lower body mass index (severe25 ± 5.8 vs non-severe 31 ± 8.4 kg/m2; p < 0.005) and fewer non-SCD comorbidities (severe 0.75 ± 1.0 vs non-severe 1.9 ± 1.8; p< 0.005). There was no difference in physical performance, falls, psychological state, SCD conditions, and number of medications by genotypes.
Of all participants, 34% reported dependence in ≥ 1 ADL/IADL. When comparing groups by ADL/IADL dependence, those who were dependent in ≥ 1 ADL/IADL had worse physical performance for all measures (gait speed, grip strength, 6-minute walk, Timed Up and Go test, and 30-Second Chair Stands). ADL/IADL dependent participants had more falls, higher PHQ-9 scores, lower MiniCog scores, more non-SCD comorbidities, and were more likely to report fair or poor vision. There was no difference in reported hearing deficits. (Table)
Conclusion
The SCD-FA was able to distinguish between known-groups by age and ADL/IADL dependence and identify deficits in adults with SCD such as falls, polypharmacy, comorbidities, and sensory deficits. Geriatric syndromes did increase with age in adults with SCD and were more common than in the general population (34% ADL dependent SCD participants vs 15% of middle-aged U.S. adults). Therefore, there is a need for early initiation of interventions to improve function and quality of life. We are currently adapting geriatric interventions for older adults with SCD. In future studies we will assess the predictive validity of the SCD-FA.
Disclosures
Strouse:Agios, Takeda, Disc Medicine: Consultancy, Research Funding.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal